Please ensure you obtain a referral before booking an appointment.
Request an appointmentRead about what your surgery will look like from fees to admissions.
Surgery with OSVFind out more about your injury, what to expect from surgery, how to get a referral and more.
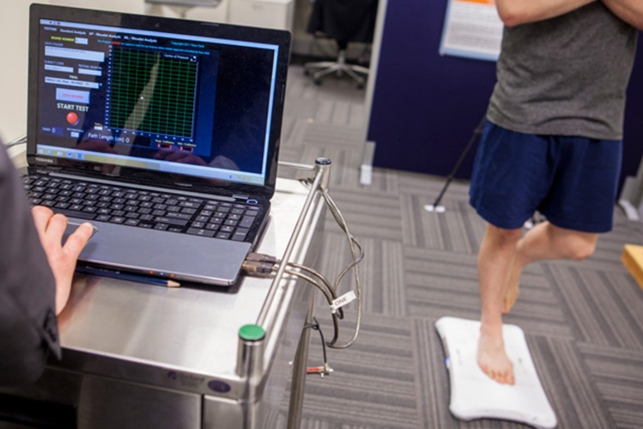
Our surgeons and research partners have a long and distinguished track record in successful research, culminating in many publications in esteemed scientific journals and presentations at meetings around the world.
If you are looking to book an appointment, please call us on