Tibialis Posterior Tendon Dysfunction, also known as Posterior Tibial Tendon Dysfunction (PTTD) or Acquired Flatfoot, is a condition where the tibialis posterior (TP) tendon, which is responsible for supporting the arch of the foot, becomes damaged or weakened.
This can lead to a collapse of the arch and a flattening of the foot, causing pain, instability, and difficulty walking. It often occurs due to overuse, injury, or aging, and can result in significant discomfort and functional impairment if left untreated.
Damage to the TP tendon can occur due to wear and tear over time, overuse, or acute trauma.
While acquired flatfoot is the most common form of tibialis posterior tendon dysfunction, there are also congenital and degenerative forms.
Acquired Flatfoot can be caused by a variety of factors, including:
Tibialis Posterior Tendon Dysfunction can lead to a range of symptoms affecting the foot and ankle, including:
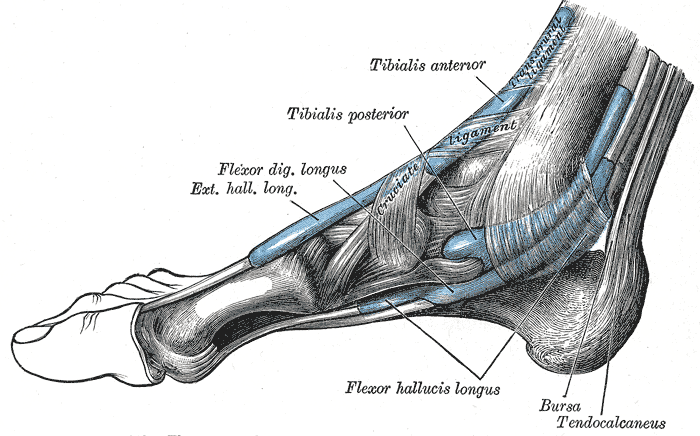
The foot is a complex structure composed of bones, muscles, tendons, ligaments, and other tissues that work together to support body weight, absorb shock, and facilitate movement. In the context of PTTD, understanding the anatomy of the foot is crucial.
One of the key structures involved in PTTD is the tibialis posterior (TP) tendon. This tendon originates from the back of the tibia (shinbone) and fibula (smaller bone in the lower leg) and runs down the inside of the ankle, passing behind the medial malleolus (the bump on the inside of the ankle). The TP tendon then inserts into multiple bones of the foot, including the navicular bone and several cuneiform and metatarsal bones.
The primary function of the TP tendon is to support the arch of the foot and control its inward position during walking and other weight-bearing activities. It helps maintain the stability and alignment of the foot’s structure, preventing excessive flattening of the arch and inward rolling of the foot (pronation).
Non-surgical treatments for PTTD offer options to ease discomfort and aid healing without surgery.
Physiotherapy uses exercises and techniques to improve muscle strength and foot function. Additionally, orthotic devices like arch supports, ankle braces and custom-moulded splints provide support, while footwear adjustments and activity modifications help reduce strain. Painkillers, including medication and therapies like ice or heat packs, complement these treatments.
Non-surgical options are suitable for mild forms of the condition however, if symptoms persist or worsen, surgery may be recommended.
Surgery typically involves removing damaged tissue from the TP tendon and surrounding structures, and repairing the damaged TP tendon. It often needs to be strengthened by using another tendon, flexor digitorum longus (FDL).
To enhance the biomechanics of the tendon transfer, a procedure known as calcaneal osteotomy is performed. This involves moving the heel bone inward towards the foot’s centre and securing it with a screw. Furthermore, a plug is inserted into the outer portion of the foot (sinus tarsi) to support the arch. Typically, the plug and screw are removed in a follow-up operation once the transferred tendon has sufficiently strengthened, usually around 6 months after the initial surgery. This procedure is often performed as a day case operation, and recovery is generally quick.
In advanced cases where multiple foot joints have become arthritic, a triple fusion procedure may be necessary. This involves stabilising and fusing three specific joints (subtalar, talo-navicular, and calcaneocuboid) using screws and bone grafts taken from either the heel or the hipbone.

These notes from OrthoSport Victoria are for educational purposes only and are not to be used as medical advice. Please seek the advice of your specific surgeon or other health care provider with any questions regarding medical conditions and treatment.
If you are looking to book an appointment, please call us on